Pubic Bone Pain Treatment in Dallas, Frisco, Prosper, and Wylie, TX
Pelvic Bone Pain and Pubic Bone Pain, Osteitis Pubis
Pelvic Pain Treatments in Dallas
Pelvic pain can happen to both men and women. This pain may stem from abnormalities in organs, infections, or the pelvic bone, itself. When women have pelvic pain, especially chronic pelvic pain, we have reason to believe it may be in relation to her reproductive system.
Treatment of pubic or pelvic pain will depend on the cause of the pain.
If you experience pelvic bone pain, one possible explanation is osteitis pubis. This condition has the potential to cause pain in the pelvis and groin area. Many times, athletes receive this diagnosis after playing certain sports. Osteitis pubis is basically inflammation of the pubic symphysis, or the joint of the two pelvic bones where they join at the front of the pelvis. This pubic symphysis is a thin joint with, normally, very minimal motion. It holds the two pelvic bones together in the front, while the sacrum connects them in the back.
At SPORT Orthopedics + Physical Therapy, our Dallas orthopedic surgeons plan your personalized treatment in a way that lets you focus on your recovery. We identify the source of your pain, then utilize state-of-the-art treatment practices that focus on restoring your range of motion and quality of life.
Depending on your symptoms and your diagnosis, our treatment options range from physical therapy to medications to possible surgery. If you’re experiencing osteitis pubis, call SPORT at 469-200-2832 to schedule your appointment with our orthopedic specialists.
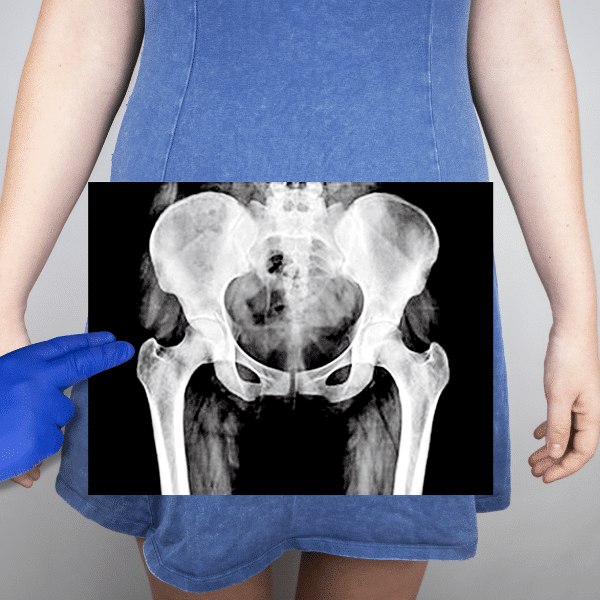
Pubic Bone Anatomy
The pubic bone is a key component of the human pelvis, forming part of the hip bone structure. It is situated anteriorly at the base of the pelvis and plays a crucial role in supporting the pelvic organs and providing attachment points for various muscles, ligaments, and tendons. Specific muscles that attach to this bony structure include the adductor muscles and lower abdominal muscles.
Pubic Body
The pubic body is the central, flattened portion of the bone that forms the front of the pelvis. It meets its counterpart from the opposite side at the symphysis pubis, a cartilaginous joint that connects the two pubic bones.
Superior Pubic Ramus
Above the pubic body lies the superior pubic ramus, which extends outward and slightly upward from the body, forming part of the pelvic brim. This portion contributes to the acetabulum, the socket of the hip joint.
Inferior Pubic Ramus
The inferior pubic ramus extends downward and inward from the pubic body, completing the arc of the pubic bone. The surrounding muscles and soft tissues attach to the inferior pubic ramus to aid with pelvic biomechanics.
Pubic Symphysis
The pubic symphysis, although fibrous and flexible, helps to transmit forces between the two sides of the pelvis, contributing to its overall strength and resilience during activities such as walking, running, and bearing weight.
Why Does My Pelvic Bone Hurt?
A multitude of different conditions can contribute to pelvic pain, some of which are mild and some of which are severe. In order to determine the source of your pain, we recommend scheduling an appointment with one of our SPORT specialists as soon as possible. First, we will ask you about your symptoms, pain level, and past medical conditions. We also perform physical exams and offer related tests to perform a proper diagnosis.
Pubic Bone Stress Injury
A pubic bone stress injury typically occurs due to repetitive stress or overuse of the pelvic region, often seen in athletes engaging in activities like running or jumping. Such stress can lead to microfractures or inflammation in the pubic bone and surrounding tissues. As a result, individuals may experience groin pain, which can range from mild discomfort to severe and debilitating pain.
The repetitive strain on the pubic bone can cause irritation, inflammation, and even structural damage, resulting in localized pain that worsens with activity and may persist even at rest. Additionally, the inflammation and tissue damage can stimulate pain receptors in the area, further contributing to the sensation of pain.

Pelvic Pain Symptoms
Pubic pain can manifest differently depending on the underlying cause of the pain. Common symptoms and pain types include the following.
- Localized pain
- Dull or sharp pain
- Pain that worsens with movement
- Pain radiating to other areas
- Pelvic pressure or heaviness
What Does Pelvic Pain Feel Like?
Pelvic pain can feel different for each individual, ranging from a dull ache or pressure to sharp or stabbing sensations. It may be localized to the pelvic area or radiate to the lower back, buttocks, thighs, or groin. Some describe it as a deep, throbbing discomfort, while others experience constant, nagging pain or intermittent bursts of sharp pain.
Groin pain may worsen with certain activities like walking, standing, or sexual intercourse, and it can be accompanied by other symptoms such as changes in bowel or bladder habits, menstrual irregularities, or pelvic pressure. Pelvic pain can manifest differently between females and males due to variations in anatomy and potential underlying causes.
Pelvic Bone Pain Female
In females, pelvic pain is commonly associated with gynecological issues such as menstrual cramps, ovarian cysts, endometriosis, pelvic inflammatory disease (PID), or fibroids. Women may experience pelvic pain that varies throughout the menstrual cycle, worsening during menstruation or ovulation.
It can feel like a dull ache, cramping sensation, or sharp stabbing pain in the lower abdomen, often accompanied by other symptoms like heavy periods, abnormal vaginal bleeding, or pain during intercourse.
Pelvic Bone Pain Male
In males, groin pain may be linked to conditions affecting the genitourinary system, such as prostatitis, epididymitis, testicular torsion, or urinary tract infections. Prostatitis, inflammation of the prostate gland, is a common cause of pelvic pain in males and can lead to discomfort in the lower abdomen, groin, or perineum.
Epididymitis, inflammation of the epididymis, can cause pain and swelling in the testicles, often accompanied by urinary symptoms like burning or urgency. Testicular torsion, a medical emergency, presents with sudden and severe testicular pain along with swelling and discoloration.
Diagnostic Tests for Pelvic Bone Pain
Diagnosing pubic bone pain usually involves a thorough medical evaluation. We often begin by taking a medical history and discussing symptoms. We will then perform a thorough physical exam which may involve palpation and manipulation to evaluate range of motion. From there, we may conduct other tests to help confirm a diagnosis of the source of your pain.
Below, we list commonly performed tests that our specialists offer when diagnosing pelvic bone pain.
- Blood/urine tests
- Pregnancy tests
- Pelvic X-rays
- MRI scans
- Bone density tests
What Causes Pelvic Pain?
Pelvic pain develops as a symptom of many different conditions. As orthopedic surgeons, we’re referring to the pelvic bone, specifically, when speaking about pelvic pain.
Some of the reasons that explain pain in the pubic bone for different individuals include:
- Pinched nerves or bulging discs can sometimes lead to pelvic pain, depending on where those places are located
- Hernia
- Broken pelvic bone
- Surgery: Sometimes, surgery leads to complications. Specifically, osteitis pubis is a complication of various types of gynecological surgeries.
- Sports injury: During certain sports activities, some people overuse or overextend parts of their body.
- Pregnancy: During this period, hormonal changes might shift the gap of the bones of your pelvis in preparation for childbirth. While pregnant or after giving birth, some women develop osteitis pubis.
- Trauma: Injuries to the lower pelvic region could cause inflammation or stress on the bones which contribute to osteitis pubis.
- Rheumatological disorders: Conditions that create inflammation in the pelvic area might result in osteitis pubis.
What Can Cause Pelvic Pain When Walking?
Pain in the pelvic region occurs as a result of a multitude of conditions, including musculoskeletal, digestive, or reproductive. Some people experience worse pain as they walk around.
Many people, especially women, will experience some type of pelvic pain over the course of their lifetime. For some, this pain worsens as they walk or begin to move around.
The common causes of pelvic pain when walking include:
- Sacroiliac joint pain: This involves irritation or inflammation of the sacroiliac joint which connects your spine to your pelvis.
- Pubic symphysis dysfunction: Sometimes, this body part becomes too relaxed. This over-relaxation results in pain which could radiate down the legs.
- Osteitis pubis: This inflammation leads to soreness and pain in the pelvic area. It generally worsens with more physical activity.
- Pelvic floor muscle pain: Sometimes, the tension in the muscles surrounding the pelvis causes pain. This pain is more common in women.
What Causes Pelvic Pain When Lying Down at Night?
Pelvic pain when lying down at night can result from many conditions or injuries, including issues with the hip flexors, a sports hernia, pelvic inflammatory disease, and other issues. Other potential causes of pelvic pain when lying down include musculoskeletal issues such as pelvic floor dysfunction or sacroiliac joint dysfunction.
How Is Pelvic Pain Treated?
The treatment options for pelvic pain will depend on what’s causing it. At SPORT Orthopedics + Physical Therapy, we’re able to treat any issues that stem from muscle problems or bone injuries.
How to Relieve Pubic Bone Pain
We often take a diagnostic and therapeutic approach when it comes to addressing the cause of the pain. Initially, resting and avoiding activities that exacerbate the pain, such as running or jumping, can help reduce strain on the pubic bone and surrounding structures. Applying ice packs to the affected area for 15-20 minutes several times a day can help alleviate inflammation and provide temporary relief from pain.
Physical therapy plays a crucial role in managing pubic bone pain by strengthening the muscles around the pelvis and improving flexibility and biomechanics. A physical therapist may recommend specific exercises to target the pelvic muscles, stretches to improve flexibility, and techniques to correct any postural or movement imbalances contributing to the pain.
In cases where conservative measures do not provide sufficient relief, more advanced interventions may be considered. This may include corticosteroid injections into the pubic symphysis to reduce inflammation and alleviate pain, or in rare cases, surgical interventions such as pubic symphysis stabilization or decompression to address structural abnormalities or instability contributing to the pain.
Pelvic Bone Pain Could Be Osteitis Pubis
What Is Osteitis Pubis?
This condition consists of inflammation of the pubic symphysis, which leads to pain. In general, this condition affects mostly young athletes. The injury itself results from overuse and occurs at the front of the pelvis along the pubic symphysis joint. This joint consists of the two pubic bones, the capsule of the joint, and the fluid within the joint.
Osteitis Pubis Risks
Several activities increase one’s risk of developing osteitis pubis, which we outline below.
- Sports such as soccer or football
- Long-distance running, fencing, ice hockey, and weightlifting
- Poor strength and flexibility
- Medical history of osteitis pubis
- Previous injuries or sprains to the pelvis
- Loss of motion or stiffness of the hip
- Previous injury to the hip
How Long Does Osteitis Pubis Last?
How long the pelvic pain is associated with this depends almost entirely on the severity of your injury. On average, most people experience a recovery period of anywhere from two to three months. After this period of time and a green light from your doctor, you may resume your normal physical activity. During your recovery period, we encourage you to seek out activities that put less strain on your pubic symphysis. For example, if you enjoy running, you could substitute that for swimming.

Once you recover and return to your normal level of physical activity, rest after each exercise. Consider taking a day or two off between sessions in order to prevent the same injury from happening. Additionally, we recommend warming up with stretches and light exercise before moving on to the more strenuous activities. While osteitis pubis can be painful, you have the power to mitigate this pain with proper rest and pain relief practices.
What Are the Osteitis Pubis Symptoms?
For the most part, symptoms of osteitis pubis are similar to any other injury associated with pelvis bone pain. Patients complain of pain in the front of their pelvis, which may or may not radiate to the groin area, lower abdomen, or inner thigh area.
Pain is typically one-sided and increases with activities such as running, pivoting your leg, climbing, lying on one side, etc.
Certain symptoms commonly accompany osteitis pubis and can help in its diagnosis. These include:
- The pelvis area is tender to the touch.
- You feel pain in your lower abdomen.
- Whenever you cough, sneeze or use the muscles of your abdomen, you feel pain.
- When you stand up or walk, you hear a clicking or popping sound.
- You have a loss of mobility and flexibility or experience weakness.
- You experience fever or chills.
How Would You Treat Osteitis Pubis?
In general, this condition resolves after a long enough period of rest. It does not require surgery or medications, except over-the-counter medications for pain or discomfort. The most important step is avoiding activities that exacerbate the problem. If you engage in activities that cause pain for the area, your recovery time will lengthen.
We recommend an ice pack application to the area for 20 minutes every three to four hours. In more severe cases, we might suggest a corticosteroid injection in order to reduce inflammation and ease your symptoms.
Physical Therapy
We often recommend physical therapy as an initial treatment of osteitis pubis. Physical therapy is a cornerstone in the treatment of osteitis pubis, a condition characterized by inflammation of the pubic symphysis and surrounding structures.
Through targeted exercises and techniques, physical therapy aims to strengthen the muscles around the pelvis, improve biomechanics, and reduce strain on the affected area. A physical therapist may prescribe a combination of strengthening exercises for the pelvic floor, core muscles, and hip stabilizers to enhance stability and support.
Additionally, stretches, strengthening exercises, and manual therapy techniques can help alleviate muscle tightness, relieve pain, and improve flexibility, reducing pressure on the pubic symphysis. By addressing any underlying muscle imbalance and promoting optimal healing, physical therapy plays a vital role in managing osteitis pubis and facilitating a return to pain-free movement and function.
Surgical Treatment
Surgical treatment of osteitis pubis is typically considered when conservative treatments have failed to provide relief and there are severe structural abnormalities or instability contributing to the condition. Surgical interventions may involve procedures such as pubic symphysis stabilization or decompression, aimed at addressing the underlying pathology and restoring normal biomechanics of the pelvis.
Pubic symphysis stabilization may involve the use of screws, plates, or other fixation devices to reinforce the stability of the pubic joint, while decompression techniques aim to alleviate pressure on the affected structures. Surgery for osteitis pubis is generally approached with caution due to the risks involved. In sports medicine, surgery is generally considered when other conservative measures have failed to alleviate the patient’s pain.
Chronic Pelvic Pain Syndrome
We’ve already discussed the definition of pelvic pain. What makes this chronic is the amount of time that a person is in pain. Typically, we’d say that chronic pelvic bone pain is a pain that lasts more than 6 months.
This may be just a mild ache, or acute pelvic pain, that comes and goes. For some, pelvic pain is a steady and severe pain that makes everyday life difficult.
CPPS Symptoms Male and Female
In males, CPPS is often synonymous with chronic prostatitis/chronic pelvic pain syndrome. The primary symptoms include pain or discomfort in the pelvic region, which may extend to the groin, perineum, testicles, and lower back.
Other symptoms can include urinary issues such as urgency, frequency, and pain during urination, as well as erectile dysfunction or pain during or after ejaculation, reflecting the involvement of the prostate and surrounding tissues.
In females, chronic pelvic pain syndrome encompasses a broader spectrum of symptoms and potential underlying conditions, given the complexity of the female reproductive system. Women may experience menstrual irregularities, pain during menstruation, or pain during sexual intercourse.
Pelvic pain may also be associated with conditions like endometriosis, where tissue similar to the lining of the uterus grows outside it, ovarian cysts, or pelvic inflammatory disease (PID). Other symptoms in women can include urinary frequency, urgency, hip pain, lower abdominal pain, and bowel movement discomfort.
What Causes Chronic Pelvic Bone Pain?
Chronic pelvic pain causes can include scar tissue in the pelvic region after surgery or infection, bowel disease, or overall problems with your muscles, joints, and ligaments in the pelvis, hips, or lower back.
Chronic pain, for females, can be attributed to the reproductive system.
Pubic Bone Pain and Osteitis Pubis Treatment in Dallas
At SPORT, we work hard to identify the source of pain for our patients, and use modern therapeutic techniques to restore their range of motion. Depending on your body, your diagnosis, and its severity, we utilize various forms of treatment. These treatment options include physical therapy, medications, injections, or even surgery in some cases. If you experienced or are experiencing pubic bone or pelvic pain, call today at 469-200-2832 to arrange your consultation with one of our orthopedic specialists.